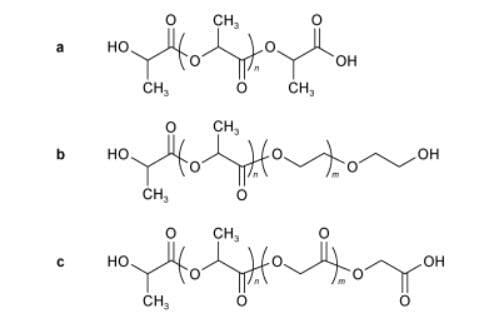
Polylactic acid (PLA) is a common bio-based polymer material, which is used in the preparation of wound dressings due to its excellent biodegradability, biosafety and easy modification. In addition to pure PLA (structure as in Fig. 1a) which has been used in wound dressing research, common PLA-PEG (structure as in Fig. 1b) and poly(lactic acid-glycolic acid) (PLGA, structure as in Fig. 1c) as well as more modified PLA have attracted much attention in this field.
Pure PLA fiber film can be used as a wound dressing as well as cotton gauze. Yagi et al. in Japan compared the hemostatic properties of a nonwoven PLA cloth developed by Toray Industries in Japan and a common rayon gauze used as a wound dressing. When the two dressings were applied to the liver sections of mice, it was found that the nonwoven PLA cloths with fiber diameters as low as 1 μm were softer than the rayon gauze with fiber diameters of about 12 μm and adhered to the wound surface more easily. More importantly, the mean hemostasis time and mean bleeding volume of the nonwoven PLA cloths were only 270 s and 0.7 g, respectively, compared with 495 s and 2.1 g for the rayon gauze. In addition, significantly better erythrocyte adhesion on the nonwoven PLA cloths than on the rayon gauze was also observed under electron microscopy, suggesting that pure PLA nonwoven fabrics can be used as hemostatic materials for incompressible hemorrhagic sites, such as minimally invasive surgery of the liver.
If the fiber size of the dressing is reduced from the micron level to the nanometer level, the degradation and absorption time of the PLA hemostatic material in the in vivo wound can be shortened, but it will bring the problem that the PLA dressing is easy to burst. In order to overcome this shortcoming, Okamura et al. (Japan) produced multilayered PLLA nanosheets with high adhesion and good flexibility by preparing multilayers of poly(L-lactic acid) (PLLA) alternating with sodium alginate (ALG), and then eluting the ALG layer, and the thickness of the nanosheets can be as low as 230 nm, and they can be used as a hemostatic dressing to reduce the adhesion of tissues after hepatic injury.
Porous PLA membranes made by Jianxun Ding et al. at the Changchun Institute of Applied Chemistry, Chinese Academy of Sciences, by physically loading 10 wt% of atorvastatin on pure PLA, could prevent fibrin bridging between the damaged tissues and the surrounding tissues, and also prevent peritoneal adhesions, which could prevent common postoperative complications such as organ dysfunctions. Physical loading of conventional hemostatic drugs not only prevents tissue adhesion, but also improves the hemostatic effect of PLA. Gong Guifen et al. from Harbin Institute of Technology loaded a PLA nonwoven dressing with polysaccharides extracted from the traditional Chinese medicine Bletilla hyacinthina, and the resulting dressing showed a bleeding time of 19 min and a blood loss of 2 mL in a rabbit ear artery hemorrhage model, compared with up to 60 min and 7 mL, respectively, in the saline control group.
In Germany, Schneider et al. physically blended poly(L-lactic acid-co-racemic lactic acid) with epinephrine (AD) and tranexamic acid (TA) hemostatic agents, respectively, to make a thin and soft electrospun fiber membrane dressing. Test results showed that AD and TA could be loaded on the dressing up to 20 wt% and 50 wt%, respectively, with release rates of 50% and 85%, respectively. The dressing has a tensile strength of more than 14 MPa, low cytotoxicity, fast hemostasis, and is particularly suitable for ENT surgery where the surgical access is small and the wound dressing is difficult to be fixed. Recently, it has been shown that pure PLA fibers loaded with Ag+ ions from a three-dimensional porous metal-organic skeleton can also sustainably kill bacteria such as EC and SA, and significantly accelerate the healing rate of infected wounds in in vivo experiments in rats.
Based on PLA fibers, other shapes of hemostatic materials can be produced. For example, Lee et al. (Korea) produced a gel particle by coating hyaluronic acid-ferric chloride mixture on electrospun PLA fibers. The gel particles can be targeted like platelets under the action of an external magnetic field to aggregate at the bleeding site, generating a stable artificial thrombus, and can increase the modulus of the thrombus by 300% and the hardness by 50%, which is similar to the effect of fibrin in increasing the strength of the thrombus, thus contributing to the process of hemostasis.
Lavik et al. (USA) developed a hemostatic nanoparticle by directly using pure PLA particles as the core and adhesive peptides as the shell. Compared with the blank group, the particles could reduce the bleeding volume of the wound and increase the survival rate of the injured mice. More importantly, the particles could maintain the original spherical powder of 100-500 nm after 7 d of storage at 50 ℃, and could still effectively stop bleeding and improve the survival rate in the rat liver injury model, indicating that the PLA hemostatic material is expected to perform well in the harsh storage and use environments, such as the battlefields of Afghanistan, where the air temperature is as high as 50 ℃.

